What to Do If You Find Someone Self-Harming

Self-harm, also called non-suicidal self-injury, is a serious and complex issue. When people are experiencing significant emotional pain, they may resort to harming themselves physically for relief. This relief is temporary, however, and the shame associated with self-harming may make emotional problems even worse. This can lead to a vicious cycle that many find it difficult to escape on their own. If you have a loved one experiencing self-harm, your supportive role could be a crucial one in their recovery.
Immediate Response Steps to Self-Harm
If you find a loved one who is currently or has just engaged in self-harm, here are some immediate steps to consider to ensure they are safe.
Stay Calm
It may feel like immediate action is needed; however, taking a moment to manage your own emotions before responding can help ensure you’re prepared to respond effectively.
Feelings of shock, fear, or anxiety are normal. Take a few deep breaths to center yourself. If you are in a state of heightened anxiety or emotion, this can add even more stress to the situation. Your calmness and composure will help de-escalate the situation and help you make good decisions. Avoid showing or expressing horror or disgust; this can be very hurtful to the person already in distress and could damage your relationship.
Assess the Situation Quickly
Next, assess the situation and identify what’s going on. Is the person actively self-harming, or have they stopped? How severe are the injuries? Is medical attention needed immediately? What is the emotional state of the person? Is the environment safe? Taking a moment to get the full picture of the situation can help you determine what to do next.
Ensure Immediate Physical Safety
If the person is still self-harming, try gently intervening. Use a calm voice while you approach them, and express your concern for their safety and well-being.
Request that they hand over any objects they are using to self-harm. Avoid using force, grabbing objects, or restraining the person unless it is absolutely necessary to prevent serious harm. If the person is seriously harmed, for example, a cut that won’t stop bleeding, immediate medical attention is likely needed, such as an urgent care or emergency room. If the person isn’t responsive, can’t be moved, or is experiencing other concerning medical problems, contact local emergency medical services by calling 911.
Provide First Aid
If the person has a wound, assess for severity and provide first aid. Follow first aid best practices, such as washing your hands first to help prevent infection. Use universal precautions, such as wearing gloves if available. Stop the bleeding by using pressure with a clean cloth. Clean the wound with running water, then apply an antibiotic ointment or petroleum jelly, and cover it with a sterile bandage.
Change the covering at least once a day. For burns, run under cool (not cold) water for 10 minutes, then apply a soothing balm, such as one with aloe vera, and bandage the area. Remember to remain calm and matter-of-fact while providing care. Medical attention should be sought if all debris can’t be removed from the wound, signs of infection show (redness around the wound), or if the person has a deep wound and may need stitches and a tetanus shot.
Protect Their Privacy and Dignity
It is incredibly important to protect the privacy and dignity of the person you are concerned about. If in a crowded space, move to a quiet, private space if possible, and conceal injuries respectfully. Avoid gossiping, taking photos, or sharing someone else’s experience without their permission.
Sharing with others who don’t need or have a right to know what’s happened can cause more harm to the person who’s already hurting.
What to Say in the Moment
Comforting words can not only validate a person’s difficult experience but also de-escalate heightened emotions.
Opening the Conversation
Use a calm, non-judgmental tone to express your concern without negative emotions like anxiety or anger. Simple phrases such as "I'm here for you,” or "I care about you, and I'm worried" can help to open the conversation. Additionally, saying out loud, "You don't have to go through this alone,” can be a powerful message to someone who’s likely been experiencing mental health concerns in isolation.
Validating Their Pain
People who engage in self-harming behaviors do so to try to alleviate great emotional pain. Validating their pain and acknowledging what you see them experiencing can be a poignant message. Simply saying "I can see you're in a lot of pain” conveys empathy and concern.
Remember, the person is more than the behaviors that are concerning you. Avoid dismissing or minimizing their feelings, because beneath the outward signs, there are often intense feelings of distress and isolation.
Asking Direct Questions
Being direct is crucial to ensuring the person is supported and safe. It is important to identify if someone who has been self-harming is at risk of suicide. Don’t be afraid to get to the point. You can do this by asking, "Are you thinking about suicide?” or "Do you want to die, or do you want the pain to stop?" It’s a common misconception that asking about suicide will “give someone the idea,” but that is not the case.
Be direct when assessing for safety, but also, how you can best support them. For example, asking "How can I help you right now?" or "What do you need?" gives them the opportunity to explain exactly what they need from you in the moment.
Phrases to Avoid
Here are some phrases to avoid, along with explanations of why they can be counterproductive and harmful. This list isn’t exhaustive, but it hopefully highlights how unhelpful attitudes are to be avoided if you wish to be helpful.
- "Why would you do this?" This could frustrate or anger the person, because people often find it hard to clearly articulate why they engage in self-harm, especially during times of heightened emotion.
- "How could you do this to me/us?" or "I'm so disappointed in you" - This is an attempt to make the situation about you and your feelings, rather than on the person impacted.
- "Just stop doing it." - They likely have, and it didn’t work. This invalidates lived experience and demonstrates that you aren’t trying to understand.
- "This is so selfish," or "You're doing this for attention." - People don’t engage in self-harm behaviors as a way to be selfish or to get attention from others. This can discourage someone from seeking support and is highly invalidating.
- "You're going to regret this." - Saying something like this could be perceived as a threat or judgmental.
- "There are people with real problems." - Pain isn’t a competition, and just because other people have it worse doesn’t mean someone’s emotional experiences aren’t real.
Ensuring Ongoing Safety
Depending on the individual circumstances, ongoing support to ensure safety may be needed.
Don't Leave Them Alone
Stay with them until additional help arrives or the crisis passes. Have someone else present if possible; that way, you can take turns being vigilant and taking breaks. If the person needs continuous monitoring, do so without hovering and respect their space while staying nearby.
Remove Self-Harm Tools
Collect sharp objects, lighters, or other items that could pose a threat to their safety. Remember, most communication is nonverbal, so keep your body language gentle and relaxed to avoid conveying judgment or anger. Explain why you are doing this, and that it is a temporary safeguard to protect their health. Secure items safely, for example, by using a lockbox.
Assess Suicide Risk
People who self-harm don’t always experience suicidal thoughts. However, they are at heightened risk, which is why assessing risk is vital.
Suicidal ideation is when someone has thoughts about death or dying from suicide. Suicide planning involves thinking about or researching methods, also called lethal means, to use for suicide. Suicidal intent is when someone has thoughts about suicide, a plan for how to carry out suicide, and an intent to follow through with that plan.
Warning signs to watch out for that someone is at risk of suicide can include the following:
- Previous history of suicide attempts
- Mood swings, especially if they are sudden and drastic
- Anger or rage
- Anxiety
- Feeling unbearable emotional pain
- Hopelessness
- Feeling trapped
- Perceiving oneself as a burden
- Isolating oneself from others
- Sleeping too much or not enough
- Increased substance use
- Seeking out ways to access lethal means
- Talking (directly or posting online) about wanting to die
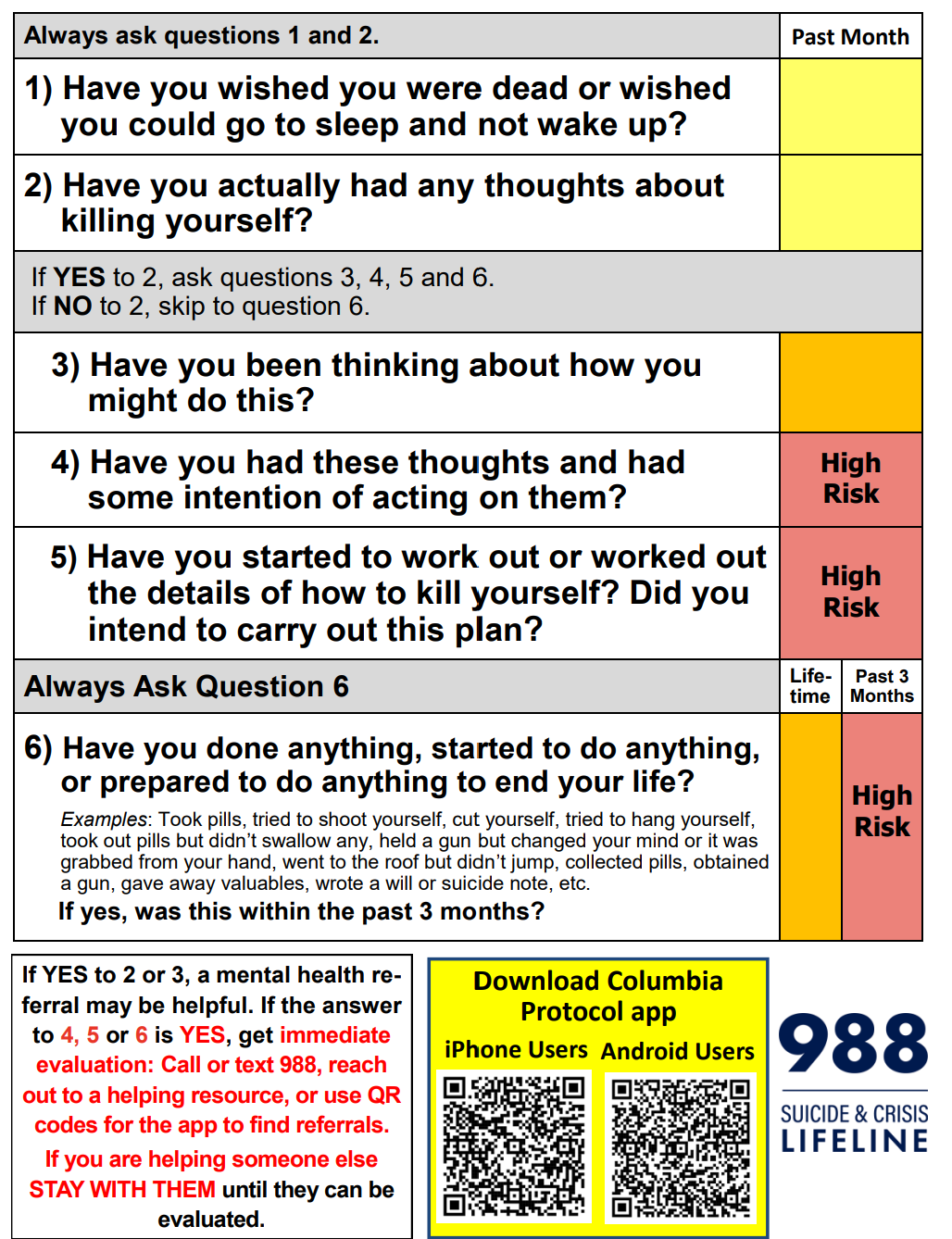
If you suspect someone may be at risk, take action. Anyone can assess for suicide risk, and we recommend using the Columbia-Suicide Severity Rating Scale (C-SSRS). This set of six questions provides guidance on the recommended steps to take based on risk level. This can help to assess if immediate psychiatric care is needed.
Create a Short-Term Safety Plan
You can support them in creating a short-term safety plan to help prevent future incidents of self-harm. This can include identifying triggers that they can avoid and coping strategies they can use to self-soothe instead of cutting. Have them identify people they can call for distraction and support.
Offer to assist them with removing and securing any objects that could be used to self-harm. Help them identify a plan to follow up with scheduling appointments with their therapist. Check in on them during the next few days and weeks following the incident to show your support and concern.
Getting Professional Help
In some instances, getting support from professionals is the best course of action. Here are a few situations where that could be the case.
When to Seek Emergency Medical Care
If the person experiences any of the following, calling 911 or going to the nearest emergency room is advised:
- Deep or gaping wounds
- Heavy bleeding that won't stop
- Wounds on the face, neck, chest, or abdomen
- Signs of infection
- Burns covering large areas
- Head injuries
- Loss of consciousness
The 988 Suicide and Crisis Lifeline can be a valuable resource to use in cases where the person’s health and safety aren’t in immediate danger. If needed, they can help link you up with local mobile crisis teams and emergency psychiatric treatment resources. People can call, text, or chat online 24/7 to reach professional support. The Crisis Text Line is another alternative, and can be reached by texting HOME to 741741.
Involving Parents or Guardians (for Minors)
If the person experiencing self-harm is a minor, this can add to the complexity of the situation. Getting their parents or guardians involved is typically advised. Don’t make promises you can’t keep, and avoid making a promise to keep the self-harming a secret.
There are cases in which youth are negatively affected by their family; in such circumstances, consult other trusted adults and professionals, such as a school counselor, to identify the steps to take. Mandatory reporting laws and obligations vary by state, and in many states, it is required that everyone report suspected child abuse to the local child protective services.
Connecting with Ongoing Mental Health Care
One way you can support the person is by helping them find a therapist who specializes in treating self-harm. Additionally, several types of therapy have been shown to be effective treatment options, including cognitive behavioral therapy, dialectical behavior therapy, mindfulness-based therapies, and family and group therapy. There are currently no medications shown to treat self-harm.
However, if the self-harm behaviors are connected to a mental health condition, treatment of that condition - with medication - will likely help to improve the self-harm as well. There are various levels of care that could be an option. Weekly individual therapy is considered outpatient treatment, as are other programs, including intensive outpatient programs (IOP) and partial hospitalization programs (PHP).
Crisis stabilization units and inpatient treatment for self-harm are typically offered for those experiencing more severe injuries or co-occurring issues like suicide risk. Attending support groups and having support from others can also be very healing.
Navigating Insurance and Costs
Many people can access mental health treatment by using their health insurance. The Mental Health Parity Act played a key role in expanding equal coverage for behavioral healthcare.
Community mental health centers offer treatment to people with state-funded insurance plans, private insurance, and many states have safety net programs that fund services for people without insurance. If the person is a child or teenager, school-based therapy services may be available.
Additionally, most therapists these days see clients virtually, so if getting to and from a therapist’s office isn’t possible, virtual care can help make getting therapy more accessible.
Frequently Asked Questions
Here are some answers to commonly asked questions about self-harm.
Is self-harm a mental illness?
Self-harm isn’t a mental illness in and of itself. It is a diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM) published by the American Psychiatric Association. Not all DSM diagnoses are considered to be mental health conditions. Self-harm is often associated with some mental health conditions and suicide risk.
Should I hide all sharp objects?
Safely storing all objects that could be used to self-harm is recommended for some time after an incident of self-harm or if the person is in a more vulnerable state.
What if they make me promise not to tell?
Avoid making promises you can’t keep, while reassuring them that you won’t disclose what happened to anyone unless they need to know.
Takeaway
Recovery from self-harm is possible. If you or your loved one is looking for mental healthcare for self-harm recovery or crisis support and prevention, reach out to us at Willow Health today. We offer same-day or next-day appointments with both a psychotherapist and a psychiatric medication clinician, who can assess your needs and identify a plan for individualized care.
Sources
About the Protocol - The Columbia Lighthouse Project
Self-harm | National Alliance on Mental Illness (NAMI)
Self-injury (Cutting, Self-Harm or Self-Mutilation) | Mental Health America
Self-injury/cutting - Diagnosis and treatment - Mayo Clinic
Cuts and scrapes: First aid - Mayo Clinic
Burns: First aid - Mayo Clinic
Stanley-Brown Safety Planning Intervention
Diagnostic and Statistical Manual of Mental Disorders (DSM) | Psychiatry Online
This article is provided for educational purposes only and is not to be considered medical advice or mental health treatment. The information contained herein is not a substitute for seeking professional medical advice for health concerns. Use of the techniques and practices outlined in this article is to be done cautiously and at one’s own risk, and the author/publisher is not liable for any outcomes a reader may experience. The author/publisher is not liable for any information contained within linked external websites. If you are experiencing a life-threatening emergency, please call 911 or the Suicide and Crisis Lifeline at 988.

